
Knee Arthroscopy
Knee arthroscopy is a keyhole procedure of the knee that can be used as a diagnostic tool or to treat a variety of pathology/conditions within the knee accurately. Common reasons for an arthroscopy are:
Meniscal injury – the menisci are two semi-lunar discs of fibrocartilage that sit between the bones (femur and tibia) of the knee joint. They act as shock absorbers and can be injured by twisting injuries of varying energy. The injury is commonly a tear which does not heal naturally and thus in the majority of patients, continues to be symptomatic. The treatment usually involves “trimming” of the tear back to a healthy and stable portion of the meniscus. In some circumstances, it may be possible to repair the torn meniscus, but the success of this is dependent on a number of factors (age of patient, type of tear, location of tear, quality of meniscal tissue).
Articular cartilage injury/damage – this is discrete, well localised damage sustained by the cartilage that lines the surface of ends of the bones that make up the knee joint. Naturally, these are extremely smooth surfaces (friction coefficient is almost zero) and thus any disruption of the surface can cause pain and restricted function. The cartilage can become loose resulting in locking of the joint or clicking. Arthroscopy allows assessment of the extent of the damage, stabilisation of the lesion (using a shaver), removal of loose fragments, and if deemed necessary, treatment of the lesion using specialised techniques e.g. microfracture. All areas of the knee are vulnerable to this kind of damage including the under surface of the kneecap (patella).
Arthritis – this is non-discrete, more diffuse damage to the articular cartilage that occurs as a function of time (wear and tear) rather than a single traumatic or sports injury. Arthroscopy may be used to wash the joint out of loose fragments and “debris” which can offer temporary symptomatic relief. The extent and grade of arthritis can be accurately assessed which can then be discussed along with further pertinent treatment options.
Biopsy – each joint has a lining or capsule (synovium), which can become inflamed for a variety of reasons. It is often necessary to take a sample (biopsy) of the synovium which is sent for further investigation, to aid in making the diagnosis.
These are the most common reasons for knee arthroscopy and Dr. Shiva is happy to discuss options available for your ailment and this varies on a case to case basis .
Will I need any tests/scans?
It is likely that X-rays and MRI will be requested for most knee injuries. Please see Surgery FAQs if you will need any other tests e.g. blood tests before your surgery.
How is it done?
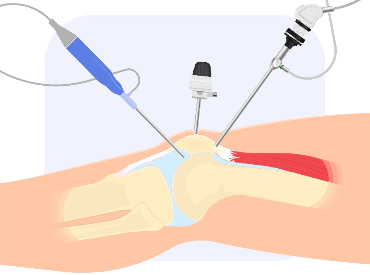
The operation is usually carried out under spinal / general anaesthetic. Two small incisions (portals) of less than 1cm are made at the front of the knee to allow the surgeon to introduce the arthroscope (fibre-optic camera) and other instruments into the joint. Very occasionally an extra portal is required. The procedure can last between 20 – 60 mins depending on what Dr Shiva has to do. At the end of surgery Dr Shiva injects local anaesthetic and sometimes a lubricant in the form of Hyaluronic acid into the knee to help minimise post-operative discomfort. A stitch is used to close each portal and waterproof dressings applied. A bandage will be then applied around your knee to provide pressure bandaging and to avoid any forms of post operative bleeding.
Can I go home the same day?
More often than not, as with most arthroscopic surgery, this is a day case procedure. Occasionally an overnight stay is advised depending on post- operative comfort levels and time of day of the surgery.
What about after the operation?
You will see a physiotherapist before discharge to be instructed on crutch use and simple exercises to carry out in the short term. Crutches are advised for several days to several weeks depending on the surgery performed. You will be prescribed analgesia to take home and Dr Shiva strongly advocates its use to keep pain to a minimum; it should be noted that pain is more difficult to control if allowed to establish itself. Dr Shiva recommends the regular application of ice as an adjunct to relieve pain and swelling in the acute post-operative period. You will see Dr Shiva two weeks after surgery for a wound check (and stitch removal) and a physiotherapy program will ensue thereafter which is paramount to the success of the operation. You are likely to have been seeing a physiotherapist before the operation and Dr Shiva will liaise with him/her in detail to advise on the post-operative exercise program.
What are the potential complications?
All surgery carries a risk. Specific risks to knee arthroscopy are:
Infection – this can be either superficial (portals) or within the joint.
Thrombosis – a clot in the deep veins of the lower limb. The risk is minimised by early mobility if possible. Oral contraceptive pills and HRT, which are known to increase risk, should be stopped before surgery.
Bleeding – this may require a return to the operating room for removal of blood clots and to stop the bleeding.
Stiffness – It is very important that some mobility of the knee is maintained after surgery. The physiotherapist will advise on simple exercises that can be carried out at home. Mr Patel also recommends that you take regular analgesia and use ice (see Surgery FAQs) for more information on how to help minimise post-operative discomfort and facilitate early movements.
Residual symptoms – unfortunately, no guarantees can be offered regarding curing your symptoms, despite the surgeon’s best efforts. In this case, further management and treatment options will be discussed with you.
